The Overlooked Connection Between Mold and Lyme disease
When it comes to chronic illness, the complexity of symptoms can often make it challenging to pinpoint the underlying cause. I have observed that many individuals coming into my practice suspect they are dealing with Lyme disease when, in fact, mold exposure may be the actual culprit. Both conditions can present with similar symptoms, making diagnosis a complicated task. Below I will aim to shed light on the relationship between mold exposure and Lyme disease and how to differentiate between the two.
Lyme Disease: A Quick Overview
Lyme disease is a tick-borne illness caused by the bacterium Borrelia burgdorferi. Its symptoms can range from fever, fatigue, joint pain, and headache to more severe complications like neurological disorders. A study published in the journal Clinical Microbiology Reviews outlines how Lyme disease is one of the most misunderstood and controversial illnesses, often leaving patients in a diagnostic limbo (1).
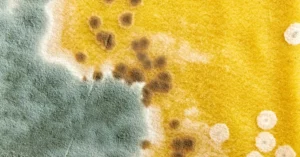
Mold Toxicity: A Stealthy Perpetrator
Mold toxicity is the result of prolonged exposure to toxic molds present in damp or poorly ventilated environments. This type of illness is also called Chronic Inflammatory Response Syndrome (CIRS).
Symptoms can vary greatly, but often include cognitive impairment (brain fog), fatigue, headaches, psychiatric symptoms, joint pain, and a compromised immune system. According to research in the International Journal of Environmental Research and Public Health, mold toxicity has been linked to a variety of chronic health conditions and should be considered a public health concern (2).
Mold illness/CIRS is often misdiagnosed because its symptoms can be similar to other conditions. Chronic fatigue, fibrobyalgia, multiple sclerosis, and yes, Lyme disease can all produce similar symptoms.
The Overlapping Symptoms: A Diagnostic Challenge
What They Share
Both conditions exhibit a range of symptoms that include but are not limited to:
- Extreme fatigue
- Cognitive difficulties
- Neurological issues
- Joint pain
- Immune system imbalances
The overlap in symptoms makes it difficult to distinguish between the two conditions, often leading to misdiagnosis or inadequate treatment.
Cytokine Reactions
Cytokines are small proteins that play crucial roles in cellular communication, especially in response to infections and inflammation. Both mold exposure and Lyme disease are known to trigger elevated levels of certain cytokines, which can result in a range of symptoms, many of which overlap between the two conditions.
Cytokine Reactions in Lyme Disease
Lyme disease, caused by the bacterium Borrelia burgdorferi, leads to an immune response where the body produces cytokines to fight the infection. However, in many chronic Lyme cases, this immune response can become dysregulated, resulting in an overproduction of cytokines.
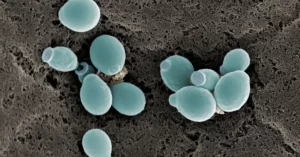
Cytokine Reactions in Mold Exposure
Mold exposure, particularly from molds that produce mycotoxins, can elicit an immune response. This response can trigger a release of various cytokines, which can create inflammatory responses in the body.
The Overlap and Interplay:
What’s especially intriguing is the overlap in symptoms between mold exposure and Lyme disease. One reason for this overlap is the similarity in cytokine reactions in both conditions. Therefore, if someone is exposed to mold while also having Lyme disease, the cytokine response can be amplified, resulting in exacerbated symptoms.
Furthermore, the weakening of the immune system due to mold exposure can make the body more susceptible to infections like Lyme disease. This dual attack on the immune system can make diagnosis and treatment more complex.
In some cases, individuals may suffer from both Lyme disease and mold toxicity simultaneously, further complicating diagnosis and treatment. A 2015 study in Toxins found that mycotoxins produced by mold can exacerbate the symptoms of Lyme disease, making it even more critical to address both issues in such cases (3).
Because exposure to mold can weaken the immune system, the body can be less capable of fending off infections, which could exacerbate Lyme disease symptoms or even make one more susceptible to contracting the disease.
How to Diagnose These Conditions:
- Lab Testing: Advanced lab tests can provide insights into the root cause of symptoms. Blood tests for Lyme disease look for specific antibodies, while tests for mold exposure may examine markers of inflammation and other immune responses.
- History and Environment: Understanding a patient\’s history and environmental exposures is crucial. Questions about the home, work environments, and outdoor activities can offer clues.
- Personalized Treatment Plans: Once the diagnosis is clear, a targeted treatment plan can be designed to address the specific cause, whether it\’s Lyme, mold, or even both in some cases.
Final Thoughts
Differentiating between mold exposure and Lyme disease can be challenging due to their similar symptom profiles. However, accurate diagnosis and treatment are essential for effective recovery. My team at Tringali Vibrant Health is committed to helping our patients navigate this intricate diagnostic maze to reach the root cause of their symptoms and find a path to vibrant health.
If you suspect you are suffering from mold exposure or Lyme disease, don\’t hesitate to seek professional medical advice for proper diagnosis and treatment.
Book a Consult Today: 561-283-1166
Sources:
- Bransfield, R.C. (2018). Neuropsychiatric Lyme Borreliosis: An Overview with a Focus on a Specialty Psychiatrist\’s Clinical Practice. Clinical Microbiology Reviews, 31(3).
- Mendell, M.J., Mirer, A.G., Cheung, K., Tong, M., & Douwes, J. (2011). Respiratory and Allergic Health Effects of Dampness, Mold, and Dampness-Related Agents: A Review of the Epidemiologic Evidence. International Journal of Environmental Research and Public Health, 8(6), 2161–2193.
- Brewer, J. H., Thrasher, J. D., Straus, D. C., Madison, R. A., & Hooper, D. (2013). Detection of Mycotoxins in Patients with Chronic Fatigue Syndrome. Toxins, 5(4), 605–617.
Request a Consultation:
Are you ready to achieve optimal, VIBRANT health? Leave your name and number below to request a consult with any of our practitioners. Or, call us at 561-283-1166 today.